If you’re anything like me (read: clumsy), you’ve probably spent your fair share of time in emergency rooms. Even if you’re blessed with grace, we all spend time in doctors’ offices at one time or another, being poked and prodded, waiting for test results, and receiving mostly reactive versus proactive care. What if we could make this process more efficient by reducing time-to-diagnosis and enabling preventative screening without taxing doctors’ time or increasing our medical bills?
Picture it: You walk into your specialist’s office, sign-in, go for your scans or tests, and boom, the physician can provide you with a diagnosis or clinical trial options then and there. While this experience is certainly not the norm today, it’s not reserved for a utopian future. In fact, medical AI makes this possible today in several settings.
Why isn’t this process widespread yet? I will share Bitfount’s hypotheses and potential solutions in the rest of this post!
First, What is Medical AI?
Medical AI is a field of AI/ML specific to using healthcare data to develop models for use in improving patient outcomes. These models can range from performing tasks such as identification of novel molecules which could be used for drug development to diagnosing a rare disease before it’s typically visible to the naked eye. The latter example, commonly referred to as a type of diagnostic AI, is the sub-field we’ll focus on together in this post.
Diagnostic AI generally represents models used to, well, infer diagnoses. For example, the field of radiology (x-rays, CT scans, etc.) presents perfect data for existing, relatively low-cost machine learning capabilities. If you’ve never broken a bone, congratulations. If you have, you likely remember sitting in a room with a big machine and a lead apron waiting for your x-rays to be done. Historically, the resulting images would be scrutinised by a radiologist, who would be charged with confirming whether your bone was in fact broken. As you can imagine, this process can be time-consuming and ambiguous depending on the type of scan, type of break, and volume of scans the radiologist must process each day. How does diagnostic AI make it easier?
In cases like that of the radiologist, diagnostic models can act as an ‘assistant,’ pre-processing scans and flagging the patients who have likely breaks. The doctor can then prioritise those scans, ensuring patients with likely breaks receive their results as soon as possible or removing false positives. The result is the doctor spends less time reviewing each scan, and the highest need patients are treated first. How are these models built?
First, a data scientist needs access to a rich data source including past images for a particular diagnosis. In a very basic scenario, a data scientist might use supervised learning to build their model, meaning they will use the data associated with each image such as demographic data on the patient, final diagnoses, and other relevant data to inform the outputs of their model. For example, if the model is for broken ankles, the data scientist will use a bunch of x-rays of ankles with details on whether the ankles are from males or females, broken or not, and what type of fracture to predict future ankle breaks. Once the data scientist has verified data quality, they build a model to read new scans and predict to a certain degree of confidence whether the new scan matches patterns seen in the previously input, or “training” data. Et voila, you have a potentially useful diagnostic AI model!
You can imagine that this approach does not need to be confined to radiology, but can be applied across many different areas of medicine. For example, Bitfount works with a fantastic team of ophthalmologists who’ve built diagnostic models to detect age-related macular degeneration from retinal scans. Now that you know what diagnostic AI is, you might be wondering why it’s not yet widespread.
Why Isn’t Diagnostic AI Used for Everything?
Diagnostic AI seems like a magical way to improve patient care, reduce care burdens on physicians, and reduce cost, but it’s important to remember it relies on data. With data come data challenges, especially when it comes to healthcare data. While diagnostic AI is used more often in practice today than one might think, it is still not a universally adopted technology as a result of several data challenges including, but not limited to:
- Data access + research limitations: The researchers with the skills to build diagnostic AI models do not always have access to the sensitive data required to build reliable models for a given diagnosis.
- Regulatory concerns: Regulation of the use of AI in medicine is still quite nascent, especially where standards differ across countries. Where there are clear guidelines, it may take significant time and resources to get a particular model or deployment method approved for use in a specific context. Ethical and accurate use regulations in relation to medical AI are crucial, but can represent a deterrent to small firms or researchers looking to commercialise their models without regulatory expertise.
- The Software/Hardware Divide: Often, data scientists and researchers with the skills to build diagnostic models lack the expertise or resources to both build and maintain software or integrate with hardware devices common in medical specialties. This approach requires builders to maintain both models and software in order to commercialise their models or research. There is often little appetite from research institutions to support what effectively become independent companies to build this software, and researchers may not wish to dedicate their time entirely to the commercialisation of a single model or set of models. Those who do make the leap to commercialisation often build fit-for-purpose medical devices or software to deploy a single diagnostic model or set of models in a specialised field. This means hospitals or clinicians need to implement several software vendors to benefit from multiple types of diagnostic models.
As with most emerging technologies, diagnostic AI’s challenges arose as a result of a lack of technical maturity, complexity in the industry (in this case healthcare), and market education. The good news is with new technologies, we can accelerate the adoption of diagnostic AI — Here’s how Bitfount plans to tackle the challenges.
Distributed Data Science in Diagnostic AI
Bitfount’s hypothesis in relation to why diagnostic AI has not yet been widely adopted is two-fold:
- The healthcare data for better diagnostic models exists, but is difficult to access at scale by data scientists with the necessary skills to build models due to data sensitivity.
- Of those data scientists who do have access to the right data, there exists only a small subset of data scientists willing or able to build companies around commercialising their models. There is a larger pool of data scientists wishing to commercialise their models if they had the right partner to which to “offload” the software/hardware divide.
We believe there is huge appetite for diagnostic models across several areas of the healthcare data life cycle, but the mechanisms for developing and deploying them include serious friction. How do we reduce these frictions? Distributed data science!
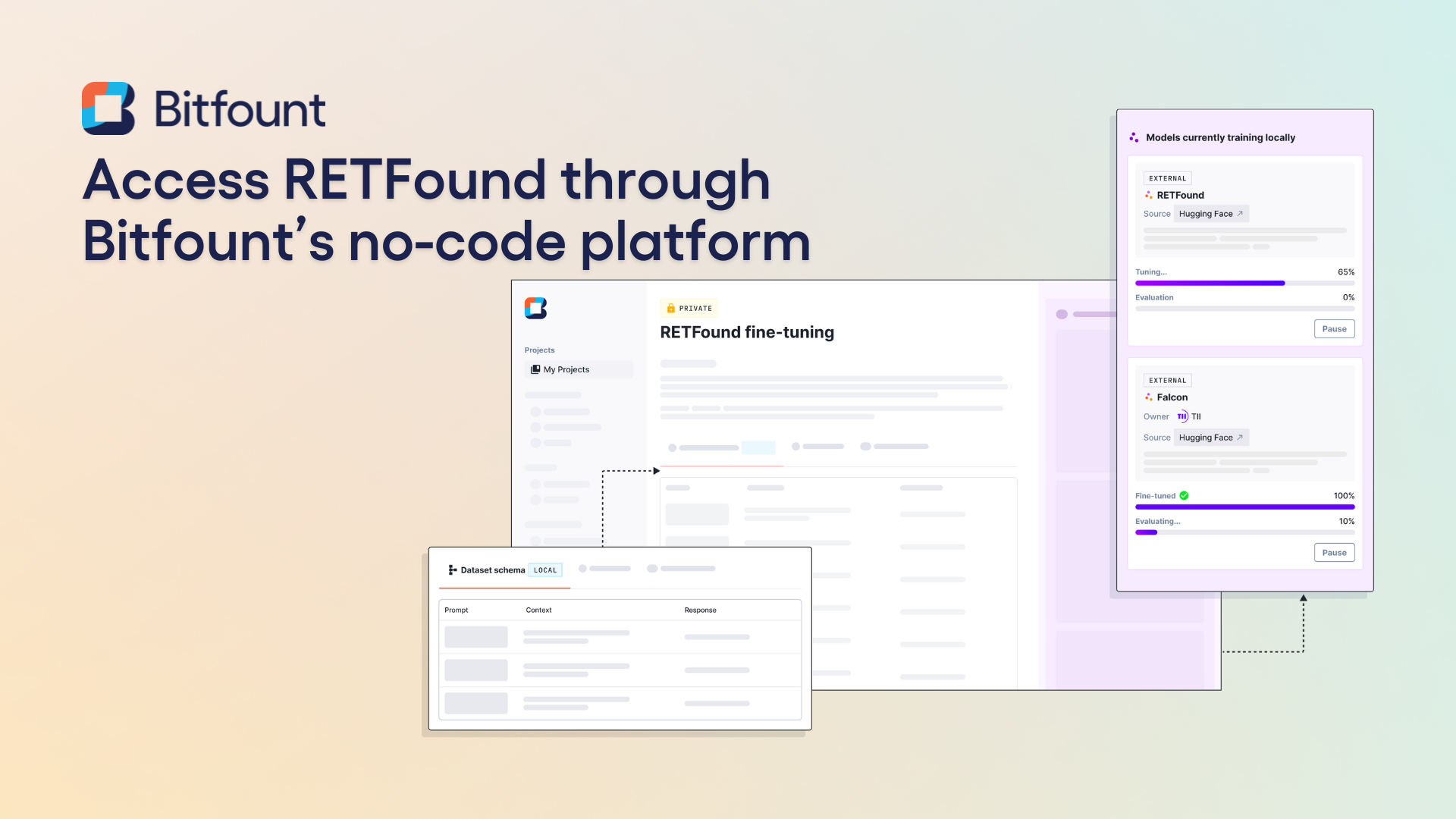
Bitfount’s distributed data science platform makes use of a federated framework such that a data scientist does not need to have a physical copy of training data to develop models or access to data used for inference to deploy models. We believe our platform addresses the existing challenges in diagnostic AI in the following ways:
- Data access: Data custodians can leverage Bitfount to enable data scientists to access data without physically transferring data or putting patient privacy at risk.
- Regulatory concerns: Bitfount’s platform handles model deployment consistently across models, meaning we can help ease the regulatory approval process based on regulatory familiarity with the platform and our own expertise.
- The Software/Hardware Divide: Bitfount allows a historically 1:1 model between model and software to become 1:many. We manage software deployment and maintenance on behalf of our modeller partners and ensure modellers are compensated for the use of their models. Hospitals and pharmaceutical companies love it because one platform can be used for many specialties or trials, while researchers and data scientists no longer need to support specialised software in order to commercialise their work.
We believe this shift to a 1:many model will unlock greater research and model development potential, while ultimately improving patient outcomes. Why shouldn’t diagnostic AI be available with ease?
Want to see our platform in action? Interested in commercialising your models? Book a demo with our team here!

.svg)
.png)

.png)
.png)